The COVID-19 coronavirus pandemic has been raging for over a year. It’s mutated into more contagious variants several times. It’s infected over 100 million people. Killed over 2 million. And apparently, preppers aren’t so crazy after all.
If you don’t have a plan of action then read ahead. I’ll describe the gravity of the situation and then cover my personal triggers.
These are events that signal that it’s time to bunker in or to get out of dodge. COVID-19 is not the flu and is proving to be an international event.
This plan of action can be applied to any pandemic, not just the current one.
Take it seriously.

Pandemics Defined
Viral and bacterial outbreaks come in three classifications: Endemic, Epidemic, and Pandemic. The difference is the persistence and the geographical area affected by the contagion.
Endemic
Endemic outbreaks apply to diseases that are a regular part of the scenery. It is always there. Malaria is a prime example. Malaria is present at all times in specific parts of the world.
Epidemics occur when a non-persistent contagion becomes widespread within a limited geographic area. The annual flu is a prime example. In early winter a strain or strains of influenza takes hold in the United States and spreads like wildfire. The flu is not typically within the population but soon spreads from shore to shore.
Pandemic
Pandemics are similar to Epidemics with one major exception. They jump geographical boundaries. The Swine Flu of 2009 was one of the more recent pandemics. It started in Mexico and jumped borders to multiple countries.
One of the key factors in a pandemic is the R0 value. This “basic reproduction number” represents the average number of people a single person will infect over their contagious period. If the R0 value is 3 then one person will infect three others. The larger the number the more rapid the spread.
So far COVID-19 has an R0 value that is hovering around 2.8. In every country, it has doubled about every 3-4 days. This has continued until extreme COVID-19 lockdown measures have been put in place.
For China, this took 22 days. For Italy 23 days.
The World Health Organization (“WHO”) listed COVID-19 as a pandemic in the middle of March (a little late folks).
Recent Pandemics
H1N1 Swine Flu
H1N1 or “Swine Flu” was first identified in Veracruz, Mexico. Within months it had spread to a total of 13 countries. From its first detection and tracking it swept through the world for over a year and a half. By late 2010 it finally burned itself out.
H1N1 was an interesting disease in that it didn’t overly affect the elderly. Historically influenza attacks those with weakened immune systems. This includes the young and the elderly.
H1N1 turned up the host’s immune system to attack the body. This resulted in more healthy people succumbing to the Swine Flu than normal.
Over 18 months H1N1 limited travel and impacted lives. The World Health Organization (WHO) tracked over 10 million confirmed cases and another 150 million suspected cases. By the end of 2010 H1N1 killed 18,500. WHO estimated that another 125,000 died from H1N1 that were not recorded.
Spanish Flu
The one we all look back to is the 1918 Spanish Flu. This is the stuff of survivalist nightmares.
The 1918 influenza pandemic was also an H1N1 variant and started in or near France. It spread throughout the world including some remote islands.
Spanish Flu worked against the host’s immune system like Swine Flu. Spanish Flu infected roughly 500 million people, or33% of the world’s population. Over 50 million died.
Epidemic to Pandemic
 As stated, the difference between an epidemic and a pandemic is the global reach. At the time of the Spanish Flu, world travel was in its infancy. By the time the Swine Flu came around, world travel was already common and rapid.
As stated, the difference between an epidemic and a pandemic is the global reach. At the time of the Spanish Flu, world travel was in its infancy. By the time the Swine Flu came around, world travel was already common and rapid.
Today, you are 12 hours from any point in the world. Millions of people fly through congested hubs every day. Even more commute on packed trains and buses.
This daily migration of humanity packs as many people as possible into confined spaces. Each minute where we pack together like sardines is an opportunity for a virus to jump from person to person.
We are lucky that we haven’t had a pandemic before now.
Crossing Shores to Your Neighborhood
Should I Worry About the COVID-19 Coronavirus?
Only you know when to take action. When to worry… that’s a different story. Worrying is a tool of fear. Make fear be your tool and tame your anxiety through information.
Information Sources
With any event this large there are too many news outlets to count. Look around and find a few that you can trust. If you can’t find any of those, find ones that you know their slant.
WHO
Let’s start globally. The WHO monitors health concerns around the globe. They track disease outbreaks and provide recommendations and material support for outbreak management. They currently produce daily COVID-19 coronavirus situation reports.
CDC
The Centers for Disease Control (CDC) is under the US Department of Health and Human Services. One of their tasks is monitoring infectious outbreaks with the potential to affect the US.
Their website provides information and situation summaries on the spread of COVID-19, including travel warnings.
If you are visually minded, Johns Hopkins has put together an amazing map that illustrates current Coronavirus COVID-19 global cases. You’ll want to bookmark these.
Doom and Bloom Medical
One of my most trusted resources is Dr. Joe Alton and Nurse Amy Alton. Medics to the prepper world, Dr. Bones and Nurse Amy can be trusted to provide timely and accurate medical information.
They cut through the hype and fear-mongering. They always provide quality information for the non-medically minded.
Doctor Bones called this one in early January. He has great foresight.
Peak Prosperity
Peak Prosperity has been known for its economic commentary. Chris Martenson has a Ph.D. in neurotoxicology and has provided a series of COVID-19 (the honey badger virus) YouTube videos that have put a laymen’s touch on this complex topic.
Related: What to Stockpile Today for Pandemic Survival: 23 Coronavirus Essentials!
COVID-19 Infectious Trends
I realize that the COVID-19 coronavirus is a rapidly evolving situation. As a result, it’s hard to define its status. What I can establish is a brief history and trends represented by the virus.
Wuhan and China
The COVID-19 coronavirus was first officially recognized in December of 2019. Within 30 days over 2,000 cases were being tracked and 50 people were dead.
The virus originated from a “wet market” in Wuhan, China. These are local farmers’ markets where fresh vegetables and meats are prepared and sold.
Early reports indicate that the virus crossed species from bats to snakes, and finally, to humans. Along the way, it picked up a few mutations that permit transmission from human to human.
Yet another mutation allows transmission in the 5-10 days that the virus is in its incubation period and is asymptomatic. In other words, you are contagious before you know you even have the virus.
The initial infections corresponded with both Christmas and the lead up to the Chinese Lunar New Year. The result was many people becoming infected and infecting others all over the world.
As soon as China recognized the severity it represented, China began a series of measures to secure the country. At the time there were already outbreaks in multiple city centers. Within days over 45 million people were quarantined as the cities were closed down.
Italy
The first big COVID-19 spread outside of China was in Italy. Two Chinese tourists in Rome tested positive and a week later a third was announced. By February 22 there were 79, and by February 29th, 1,128.
The explosive spread led to the first lockdown of 50,000 people by February 22. As of March 15th, there were over 24,000 cases and most of the country is in lockdown.
Effective Quarantine?
Only history will tell if these measures will stop the spread in its tracks. That is unlikely.
WHO has already reported many cases outside of the Chinese mainland. This includes several countries in Asia, France, Canada, and the United States.
Note: check the New York Times COVID-19 US case tracker to see if there have been any cases reported near you.
Quarantine measures are rarely 100% effective. Someone, somewhere always finds a way out.
Moreover, timing is critical. It is doubtful that the infected from the first month remained in the quarantine zone.
Remember each infected individual is contagious but not symptomatic for 5-10 days. It is highly probable that “healthy” people traveled the globe spreading the disease.
Social Distancing
We’re probably all now familiar with the term, “social distancing”. However, for many of you, that was a brand new phrase.
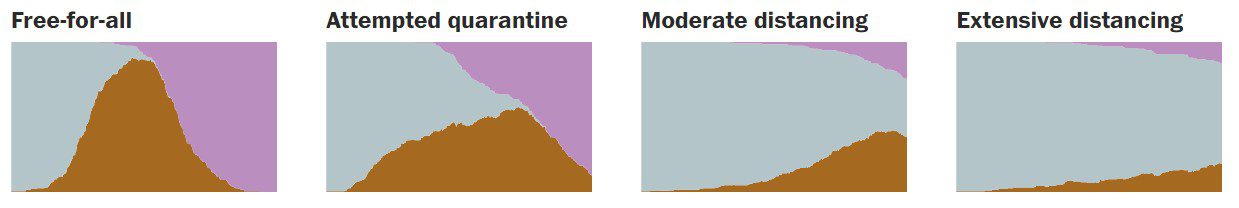
As mentioned in Chris Martenson’s video above, there is a link to a Washington Post article about the effectiveness of social distancing vs a forced quarantine.
Yes, this is just the beginning (as of this writing anyway) of an extensive disruption to our lives. But distancing ourselves from each other, for a little bit, appears to be the best way to mitigate the spread.
Disruption at Home
Speaking of disruption. My workplace, the gym, the local coffee shop are closed. Additionally, most (if not all) of our schools are closed.
We must do our best for ourselves and our family. This becomes a fine balance when action equals disruption. Taking your kids out of school, staying home from work, or completely bugging out all impact our lives significantly.
On the flip side, not acting leads to illness in the family or worse. The sick and the caregiver(s) won’t fulfill normal family duties. This leaves the others to pick up the slack.
Worse, sickness in the home brings rise to the risk of the others getting sick. There’s nothing worse than a house full of sick people… just ask my wife.
Seeking Care
Always consider the peril associated with seeking care. There may come a time when you can’t provide sufficient care. If this is the case, you’ll have to seek professional medical care.
Rule #1 of getting sick during flu season, avoid the hospital at all costs.
I admire beyond words the work of our caregivers. That being said, they are human. In times of epidemics or pandemics, the pressure to perform is unrivaled.
COVID-19 appears to be airborne. The probability of keeping the disease from spreading is zero.
Hospitals will be local epicenters of contagion. Walking through the doors puts you at risk for illness.
Hospitals won’t be the only areas of risk. Doctor’s offices and pharmacies attract the sick and contagious (but asymptomatic). If you don’t require professional medical care, consider treating minor symptoms with home remedies.
Regardless of the direction you take, you risk disruption in your life. All you can do is form the best plan possible, be observant, and establish triggers for action.
In response to the massive caseload and the inability to treat all patients Italy is triaging. Those cases that have a minimal chance of survival are not being treated. This is not a situation you want to walk into needlessly.
When Close is Too Close?
So, when is close too close? That’s the $64,000 question, isn’t it?
What I can’t do is put myself in your shoes. What I can do is share my plan. Sharing a little bit of my thought process may give you a few more data points. Use these to get past the worry and into action.
Personal Vectors
First, a little about my position. Married, kids, and I spend my 9-5 working in a corporate setting with a bunch of other office jockeys. Like most other companies 90% of the company sits at their desks. We occasionally socialize. The other 10% hit the pavement selling our goodies. About half of those travel internationally.
I occasionally get tapped to travel for demos, sales events, and training. I average between 10% and 20% of my time on the road. Half is within the US the other half is international. As I write this I’m preparing for a short international trip.
I’ll share my travel preparations another day.
From my perspective, there are three vectors for my family to get sick: 1) routine travel, 2) work, and 3) school.
Our routine travel includes going “into town” for groceries, church, and miscellaneous errands. I’ll include social events even though these are few.
The vector of work includes contact with co-workers. Each co-worker has their own vectors. Special cases are the traveling sales staff.
School is a petri dish. Enough said.
Before we look at the triggers let’s look at the specific conditions where we can get sick.
Routine Travel
We can control when and how often we go out to get the essentials. If we wanted to push it, we could go several weeks without a trip to the corner store.
The same with our other errands. I don’t have an immediate need for much.
Finally, I have no problem dialing back our social schedule if needed. Now let’s take a closer look at each.
Going to the grocery store, mall, and general shopping is one of the biggest risks. You don’t know the people or their health status.
Likewise, you can barely control incidental contact. Opportunities to wash your hands are limited and most surfaces aren’t cleaned with any regularity.
Worse yet, the COVID-19 coronavirus is airborne. This includes breathing in contagion as well as surface contact with viral particles. Especially your eyes.
Physiology lesson. Your eyes are warm, moist, and connected to your tear ducts, which vent into your sinuses. Consequently, your sinuses lead to your lungs which is where the COVID-19 coronavirus wants to be.
A single cough will send thousands of viral droplets into the air. Most will fall to the ground within a few seconds. Some will continue to float until they find you. The more people, the larger the plume of virulence.
Long story short, crowds suck.
Miscellaneous errands include entertainment (e.g. movies, restaurants, etc.), hardware store, electronics store, gas station, etc. These can be limited. Sometimes you just need a new tool or a fill-up.
In most cases, we will change to off-hour shopping. You won’t find me anywhere near a bank at noon or 4 pm on a Friday. I’ll go grocery shopping at 7 am or 11 pm to avoid crowds.
Most Walmarts are open 24 hours. If we need a cheeseburger we’ll do an early dinner at 3 pm.
March 16, 2020 Update:
With new information the above recommendations hold.
Avoid crowds and keep to yourself as much as possible. We have already seen runs on toilet paper, sanitizers of all shapes and sizes, and food. State and local governments have started to close things down and businesses are following suit.
This has resulted in large crowds forming at big box stores as well as travel centers. The restrictions put on international flights and caused a flood of travelers looking to go somewhere else. These are the easiest examples of what to avoid.
Related: Learn how to make your own DIY hand sanitizer.
Work
I, like many others, am a slave to the paycheck. The dream is to retire off grid, but it’s not in the cards yet.
Therefore, every morning I suffer through another commute. In my own car. No carpool or public transportation is available.
When I’m in the office there are no crowds and we limit personal contact. We have the occasional handshake or fist bump but that’s it. During flu season we keep to ourselves.
Most of the common areas are cleaned with regularity. Most importantly I control the area that I am in the most. My office. During flu season I clean the main surfaces weekly.
The only part of my day that is out of my control is meetings. I have no problem sitting in the back of the room.
The primary risk at work is the non-symptomatic carrier. The is the person just back for a trip, or with a sick kid that is carrying and spreading the coronavirus but doesn’t know it yet.
School
There is nothing hygienic about public schools.
As much as the staff teaches the kids to cough into an elbow and wash their hands after using the bathroom, it doesn’t happen. Packing that many teens or pre-teens into close quarters is a hygienic nightmare. It only takes one sneeze followed by overactive hormones to pollute the entire school.
Once-daily cleanings by the janitorial staff can’t keep up. There are too many opportunities for a virus to be passed around.
More than once in the past decade my children’s’ school has been closed due to too few students. This is common for other local schools.
My Triggers for the COVID-19 Coronavirus
So, we’ve covered the history and effects of the COVID-19 coronavirus. We’ve covered its potential spread around the world. Lastly, we’ve covered the potential threats in my area.
Now let’s look at establishing “go time”.
The current reality is that the COVID-19 coronavirus seems to be relatively contagious. Its estimated R0 is between 2 and 4.
The fatality rate is currently hovering between 2% and 3%.
Finally, it particularly affects the very old and very young. These are concerning factors but they aren’t exactly biblical. I will accelerate my plans if either the mortality changes or the mix of those affected skews to healthier individuals.
When will I get concerned? Glad you asked.
Considering my three vectors I have three plans of action. I’ll work those in reverse based on our life patterns.
School
I’m not shy about taking my kids out of school. Our district has computerized most of their education. Not to diminish the teachers, but way too much is taught via YouTube.
Frankly, my kids are self-sufficient enough to learn outside of the boundaries of school.
That being said, my trigger is a single case in our school or within the surrounding districts. If it’s in our town, then siblings can pass to siblings, boyfriend passes to girlfriend, etc. All of a sudden, my child is in the crosshairs.
If it’s in a neighboring town we’re done too. School athletics and exchange programs provide opportunities to pass diseases between schools.
Likewise, kids congregate regardless of town. In my day it was the mall and the arcade. These days who knows. They find common ground and gather.
The only exception I will make to this rule is if the infected student or teacher is the direct result of out of town travel. However, the minute it’s person to person in our town. We’re homeschooling until this blows over.
Work
There’s not going to be a lot of hanging around the water cooler for me over the next month or two. Luckily, I control the majority of my schedule and I can close my office door.
For the times that I have to interact with co-workers, I can control where I sit and keep track of what I touch.
We have bottles of hand sanitizer in all common areas and I don’t need to touch too many doorknobs. I am free to wash my hands as often as I like. I do. After every meeting.
What are my work triggers? There are two. One, a suspected case in the building. Two, direct knowledge of a case in a co-worker’s children’s school or immediate vicinity (spouse, constant contact relative, etc.)
I have no problems packing up and working from home (my boss knows I’m more productive at home).
In the unfortunate event that I need to travel, I will do everything possible to skip the trip. Prior family obligations, the kid has their third appendix removed, etc. I’ll stay at home.
March 16, 2020 Update:
Again this has not come to pass. Businesses around the state have taken the initiative to close early. Social distancing has become the mantra and an office is a bad place to be.
If you have the opportunity to work remotely take it and do it now. If that is not a possibility then increase your hygiene routines and keep at least 10’ from people as much as possible.
Routine Travel
Increased Awareness
This is the toughie. When do you decide that the caseload where you travel is too much?
The impact can be large. You are deciding to forgo all non-essential travel for groceries, repair items, routine medical checkups, and entertainment.
In our case, we are already exercising elevated caution. We have changed up our shopping hours to be off-peak. We have rescheduled our immediate appointments to be as soon as possible. It was lucky that we were able to advance a pair of those appointments by a month, so they are now complete.
We have decided as a family that any cases related to travel (e.g. the person was in China and now has symptoms) are not a great concern. They are initial contact and won’t raise any personal alarms.
If there are multiple cases of person to person transfer then we are on high alert.
We will severely restrict personal travel. This includes going into town even with additional precautions. Precautions include face masks, a change of clothes upon returning, and a scrub down of hands and face.
In our rural area, this has not come to pass yet, but it will.
In the local, more urban areas, case counts have increased doubling about every 3 days. I have high confidence that it will continue to spread unchecked as the US is limited in the number of tests it has and the local infected population is higher than the numbers show.
Increase your social distance as much as possible if you have to go out. Never go out unless it is absolutely necessary.
Time for Action
Where it gets real is if there are numerous cases of active coronavirus treatment (1-2% of the population) in our state or neighboring states.
The other trigger is a confirmed COVID-19 death within our surrounding counties. This encompasses everywhere within a 60-90-minute drive.
At this point, we start our bug in planning and shut down all non-essential travel.
If we can bug out (e.g. our preferred locations are in better shape than home) we will evacuate if there are multiple deaths in the surrounding communities. Keep in mind there are several places you don’t want to be when SHTF.
I know this is a little ambiguous however, there are multiple factors to consider.
These include exact location, social separation (e.g. church member vs someone on the other side of the state), and demographics (if the death has no other complications – compromised immunity, elderly, infant, etc.), as well as the overall progression.
The short of it is we will watch and act before it’s too late.
We are prepared to bug in. We are actively topping our stores off and have made several official “Last Shopping Trips.”
The “Last Grocery List” includes durable vegetables (cauliflower, potatoes, winter squash, etc. – basically anything that will stay fresh for more than a week) and durable fruits (apples, pineapple, and the greenest bananas I can find).
This allows us to have a few fresh foods over the next month.
COVID-19 Coronavirus Plan of Action Summary
A little long-winded I know (again just ask my wife) but here is my final plan of action.
- For the moment we are staying put and have only modified our routine travel such that we are shopping in the off hours and not going out to eat as much.
- We have increased our coronavirus precautions including social distancing, washing hands, and face every chance we get.
- We will take our kids out of school if there is a single case in the district or within the neighboring schools. As a wise man once said. “School is a petri dish. Enough said.”
- I will leave work and telecommute if there is a case in the office or one of my co-workers has one of my triggers (a case in their school, or a relative with the disease).
- A multitude of cases or a death in my town or bordering towns will cause us to bug in.
- A rapid increase in cases will trigger our bug out plan.
These are not decisions we will take lightly as they will profoundly disrupt our lives. But better to be disrupted than sick or worse.
Conclusion
We all run tabletop exercises daily. Most are informal “what if” scenarios that bear little weight other than keeping our skills sharp. When it comes to a potential national crisis it’s time to get serious.
I’m not saying that the COVID-19 coronavirus has the potential to be Steven King’s “Captain Trips”. I’m also not saying that it’ll pass without affecting anyone in the reading audience.
All current signs point to it being worth of attention and potentially worthy of action. The increase in the number of cases per day. The 2% mortality rate. The supposition that it is contagious while non-symptomatic in the patient. These factors all get my immediate attention.
If these trends continue and the current assumptions prove factual then we will take a serious look at evacuation. As always, you evacuate to increase your chances of survival. If survival presents a challenge at home then we will bug out to a location where the odds are more in our favor.
I stated before that I’m not in your shoes and can’t provide qualified advice to you. What I have done is present my view of the situation, my threat matrix, and my triggers for action.
Through this view, I hope you can review and refine your plans to better arm you for a clinical action and not an emotional reaction.